Esperin
* Please be kindly noted products are not for therapeutic use. We do not sell to patients.
| Category | Antibiotics |
| Catalog number | BBF-02025 |
| CAS | |
| Molecular Weight | 839.97 |
| Molecular Formula | C39H65N7O13 |
Online Inquiry
Description
Esperin is an ester peptide antibiotic produced by Bacillus mesentericus. It has anti-gram-positive bacteria and mycobacterial activity.
Specification
| Storage | Store at -20°C |
| IUPAC Name | 2-[[2-[[16-(2-carboxyethyl)-20-methyl-10,13-bis(2-methylpropyl)-2,6,9,12,15,18-hexaoxo-7-propan-2-yl-1-oxa-5,8,11,14,17-pentazacycloicosane-4-carbonyl]amino]-4-methylpentanoyl]amino]propanoic acid |
| Canonical SMILES | CC1CC(=O)NC(C(=O)NC(C(=O)NC(C(=O)NC(C(=O)NC(CC(=O)O1)C(=O)NC(CC(C)C)C(=O)NC(C)C(=O)O)C(C)C)CC(C)C)CC(C)C)CCC(=O)O |
| InChI | InChI=1S/C39H65N7O13/c1-18(2)13-25(34(52)40-23(10)39(57)58)43-36(54)28-17-31(50)59-22(9)16-29(47)41-24(11-12-30(48)49)33(51)42-26(14-19(3)4)35(53)44-27(15-20(5)6)37(55)46-32(21(7)8)38(56)45-28/h18-28,32H,11-17H2,1-10H3,(H,40,52)(H,41,47)(H,42,51)(H,43,54)(H,44,53)(H,45,56)(H,46,55)(H,48,49)(H,57,58) |
| InChI Key | UDKIYKILOKEDQK-UHFFFAOYSA-N |
Properties
| Appearance | White Powder |
| Antibiotic Activity Spectrum | Gram-positive bacteria; mycobacteria |
| Melting Point | 238°C (dec.) |
| Solubility | Soluble in Methanol |
Reference Reading
1. Endovascular thrombectomy versus standard bridging thrombolytic with endovascular thrombectomy within 4·5 h of stroke onset: an open-label, blinded-endpoint, randomised non-inferiority trial
Peter J Mitchell, Bernard Yan, Leonid Churilov, et al. Lancet. 2022 Jul 9;400(10346):116-125. doi: 10.1016/S0140-6736(22)00564-5.
Background: The benefit of combined treatment with intravenous thrombolysis before endovascular thrombectomy in patients with acute ischaemic stroke caused by large vessel occlusion remains unclear. We hypothesised that the clinical outcomes of patients with stroke with large vessel occlusion treated with direct endovascular thrombectomy within 4·5 h would be non-inferior compared with the outcomes of those treated with standard bridging therapy (intravenous thrombolysis before endovascular thrombectomy). Methods: DIRECT-SAFE was an international, multicentre, prospective, randomised, open-label, blinded-endpoint trial. Adult patients with stroke and large vessel occlusion in the intracranial internal carotid artery, middle cerebral artery (M1 or M2), or basilar artery, confirmed by non-contrast CT and vascular imaging, and who presented within 4·5 h of stroke onset were recruited from 25 acute-care hospitals in Australia, New Zealand, China, and Vietnam. Eligible patients were randomly assigned (1:1) via a web-based, computer-generated randomisation procedure stratified by site of baseline arterial occlusion and by geographic region to direct endovascular thrombectomy or bridging therapy. Patients assigned to bridging therapy received intravenous thrombolytic (alteplase or tenecteplase) as per standard care at each site; endovascular thrombectomy was also per standard of care, using the Trevo device (Stryker Neurovascular, Fremont, CA, USA) as first-line intervention. Personnel assessing outcomes were masked to group allocation; patients and treating physicians were not. The primary efficacy endpoint was functional independence defined as modified Rankin Scale score 0-2 or return to baseline at 90 days, with a non-inferiority margin of -0·1, analysed by intention to treat (including all randomly assigned and consenting patients) and per protocol. The intention-to-treat population was included in the safety analyses. The trial is registered with ClinicalTrials.gov, NCT03494920, and is closed to new participants. Findings: Between June 2, 2018, and July 8, 2021, 295 patients were randomly assigned to direct endovascular thrombectomy (n=148) or bridging therapy (n=147). Functional independence occurred in 80 (55%) of 146 patients in the direct thrombectomy group and 89 (61%) of 147 patients in the bridging therapy group (intention-to-treat risk difference -0·051, two-sided 95% CI -0·160 to 0·059; per-protocol risk difference -0·062, two-sided 95% CI -0·173 to 0·049). Safety outcomes were similar between groups, with symptomatic intracerebral haemorrhage occurring in two (1%) of 146 patients in the direct group and one (1%) of 147 patients in the bridging group (adjusted odds ratio 1·70, 95% CI 0·22-13·04) and death in 22 (15%) of 146 patients in the direct group and 24 (16%) of 147 patients in the bridging group (adjusted odds ratio 0·92, 95% CI 0·46-1·84). Interpretation: We did not show non-inferiority of direct endovascular thrombectomy compared with bridging therapy. The additional information from our study should inform guidelines to recommend bridging therapy as standard treatment. Funding: Australian National Health and Medical Research Council and Stryker USA.
2. Comparative effectiveness and safety of non-vitamin K antagonists for atrial fibrillation in clinical practice: GLORIA-AF Registry
Gregory Y H Lip, Agnieszka Kotalczyk, Christine Teutsch, Hans-Christoph Diener, Sergio J Dubner, Jonathan L Halperin, Chang-Sheng Ma, Kenneth J Rothman, Sabrina Marler, Venkatesh Kumar Gurusamy, Menno V Huisman; GLORIA-AF Investigators Clin Res Cardiol. 2022 May;111(5):560-573. doi: 10.1007/s00392-022-01996-2. Epub 2022 Mar 16.
Background and purpose: Prospectively collected data comparing the safety and effectiveness of individual non-vitamin K antagonists (NOACs) are lacking. Our objective was to directly compare the effectiveness and safety of NOACs in patients with newly diagnosed atrial fibrillation (AF). Methods: In GLORIA-AF, a large, prospective, global registry program, consecutive patients with newly diagnosed AF were followed for 3 years. The comparative analyses for (1) dabigatran vs rivaroxaban or apixaban and (2) rivaroxaban vs apixaban were performed on propensity score (PS)-matched patient sets. Proportional hazards regression was used to estimate hazard ratios (HRs) for outcomes of interest. Results: The GLORIA-AF Phase III registry enrolled 21,300 patients between January 2014 and December 2016. Of these, 3839 were prescribed dabigatran, 4015 rivaroxaban and 4505 apixaban, with median ages of 71.0, 71.0, and 73.0 years, respectively. In the PS-matched set, the adjusted HRs and 95% confidence intervals (CIs) for dabigatran vs rivaroxaban were, for stroke: 1.27 (0.79-2.03), major bleeding 0.59 (0.40-0.88), myocardial infarction 0.68 (0.40-1.16), and all-cause death 0.86 (0.67-1.10). For the comparison of dabigatran vs apixaban, in the PS-matched set, the adjusted HRs were, for stroke 1.16 (0.76-1.78), myocardial infarction 0.84 (0.48-1.46), major bleeding 0.98 (0.63-1.52) and all-cause death 1.01 (0.79-1.29). For the comparison of rivaroxaban vs apixaban, in the PS-matched set, the adjusted HRs were, for stroke 0.78 (0.52-1.19), myocardial infarction 0.96 (0.63-1.45), major bleeding 1.54 (1.14-2.08), and all-cause death 0.97 (0.80-1.19). Conclusions: Patients treated with dabigatran had a 41% lower risk of major bleeding compared with rivaroxaban, but similar risks of stroke, MI, and death. Relative to apixaban, patients treated with dabigatran had similar risks of stroke, major bleeding, MI, and death. Rivaroxaban relative to apixaban had increased risk for major bleeding, but similar risks for stroke, MI, and death. Registration: URL: https://www. Clinicaltrials: gov . Unique identifiers: NCT01468701, NCT01671007. Date of registration: September 2013.
Recommended Products
| BBF-01829 | Deoxynojirimycin | Inquiry |
| BBF-02642 | Lactonamycin | Inquiry |
| BBF-01825 | Loganin | Inquiry |
| BBF-01826 | Deoxymannojirimycin | Inquiry |
| BBF-05862 | Epirubicin | Inquiry |
| BBF-02614 | Nystatin | Inquiry |
Bio Calculators
* Our calculator is based on the following equation:
Concentration (start) x Volume (start) = Concentration (final) x Volume (final)
It is commonly abbreviated as: C1V1 = C2V2
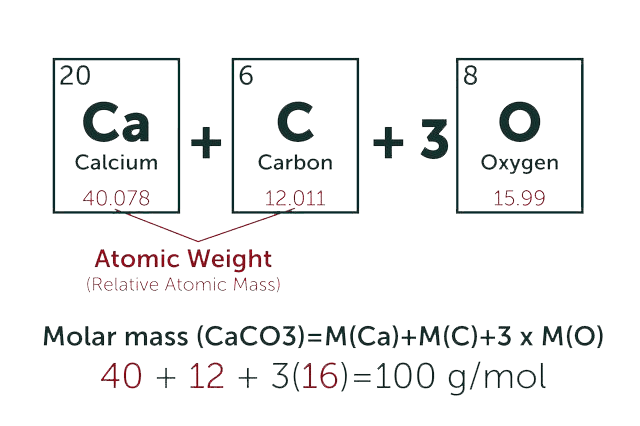
* Total Molecular Weight:
g/mol
Tip: Chemical formula is case sensitive. C22H30N4O √ c22h30n40 ╳